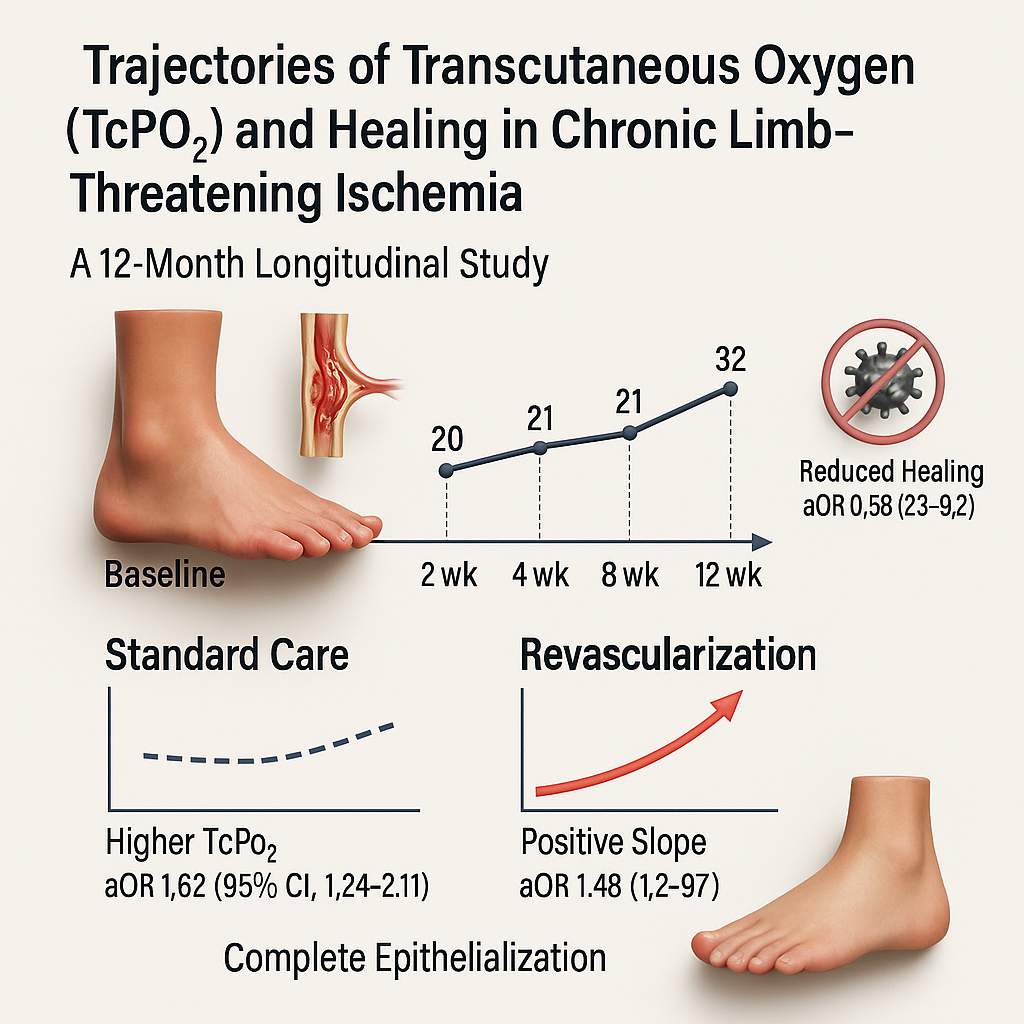
Trajectories of Transcutaneous Oxygen (TcPO2) and Healing in Chronic Limb-Threatening Ischemia: A 12-Month Longitudinal Study
DOI:
https://doi.org/10.70196/jwrt.v2i2.67Keywords:
chronic limb-threatening ischemia, peripheral arterial disease, transcutaneous oxygen pressure, cohort studies, trajectoriesAbstract
Background: Chronic limb-threatening ischemia (CLTI) remains a major global burden with high amputation risk, while evidence on using transcutaneous oxygen pressure (TcPO₂) trajectories (level + slope) to guide healing decisions is limited. Most studies treat TcPO₂ as a static threshold, not a time-updated signal that could trigger earlier escalation.
Purpose: This study aimed to estimate the association of TcPO₂ trajectories and revascularization with wound-healing probability among patients with CLTI over 12 months.
Methods: In a prospective longitudinal cohort at a Japanese hospital (Mar 3, 2023- Mar 1, 2024), we enrolled 46 adults with tissue-loss CLTI meeting guideline ischemia criteria; acute limb ischemia and non-ischemic ulcers were excluded. Standardized wound care was provided; revascularization was time-varying (from procedure date). TcPO₂ was measured at baseline, 2, 4, 8, 12 weeks, and 6, 9, 12 months. The primary outcome was complete epithelialization sustained for ≥2 visits. Discrete-time survival models estimated adjusted odds ratios (aORs) with 95% CIs, adjusting for age, diabetes, infection, albumin, WIfI ischemia grade, and smoking; sensitivity analyses included competing risks and joint modeling.
Results: Among 46 participants (mean age 71 years; diabetes 78%; CKD 41%), baseline mean TcPO₂ was 18.3 mmHg (standard care 21.2; revascularization 16.3). From baseline to Week 12, TcPO₂ rose +2.9 mmHg under standard care versus +15.8 mmHg post-revascularization. Higher time-updated TcPO₂ and positive slope independently increased healing (per 10 mmHg aOR 1.62, 95% CI 1.24-2.11; per 1 mmHg/week aOR 1.48, 1.12–1.97). Revascularization was beneficial (aOR 2.35, 1.18-4.68), while visit-level infection reduced healing (aOR 0.58, 0.36-0.92). Effects were directionally robust across sensitivity analyses.
Conclusion: Trajectory-based TcPO₂ monitoring (level and slope) identifies an early, actionable window after baseline especially post-revascularization when timely escalation can improve healing. Findings support embedding serial TcPO₂ into CLTI care and motivate multicentre evaluations of effectiveness, cost, and equity.
Downloads
References
Ariani, I., Putra Harsya, D., & Burhan, A. (2024). A comparison of the effects of contemporary dressings and 1% Povidone Iodine on the healing of diabetic ulceration: A Quasy Experiment. Journal of Wound Research and Technology, 1(1), 19–27. https://doi.org/10.70196/jwrt.v1i1.4
Arsenault, K. A., Al-Otaibi, A., Devereaux, P. J., Thorlund, K., Tittley, J. G., & Whitlock, R. P. (2012). The use of transcutaneous oximetry to predict healing complications of lower-limb amputations: A systematic review and meta-analysis. European Journal of Vascular and Endovascular Surgery, 43(3), 329–336. https://doi.org/10.1016/j.ejvs.2011.12.019
Burhan, A., & Arofiati, F. (2021). Effect of Compression Bandage on the Healing of Diabetic Foot Ulcers: A Scooping Review: 4th International Conference on Sustainable Innovation 2020–Health Science and Nursing (ICoSIHSN 2020), Yogyakarta, Indonesia. https://doi.org/10.2991/ahsr.k.210115.110
Burhan, A., Arofiati, F., Abreu Da Silva, V., & Mixrova Sebayang, S. (2023). Effect of ankle brachial index (abi) and compression therapy on diabetic foot ulcer healing. Current Diabetes Reviews, 19. https://doi.org/10.2174/1573399819666230331083420
Campbell, D. B., Shah, N., Suarez-Pierre, A., & Abularrage, C. J. (2023). The natural history of chronic limb-threatening ischemia. Seminars in Vascular Surgery, 36(3), 246–255. https://doi.org/10.1053/j.semvascsurg.2023.07.003
Castilla, D. M., Liu, Z.-J., & Velazquez, O. C. (2012). Oxygen: Implications for wound healing. Advances in Wound Care, 1(6), 225–230. https://doi.org/10.1089/wound.2011.0319
Conte, M. S., Bradbury, A. W., Kolh, P., et al. (2019). Global vascular guidelines on the management of chronic limb-threatening ischemia. Journal of Vascular Surgery, 69(6S), 3S–125S.e40. https://doi.org/10.1016/j.jvs.2019.02.016
Dua, A., et al. (2025). Contemporary outcomes in no-option chronic limb-threatening ischemia. Annals of Vascular Surgery. Advance online publication. https://doi.org/10.1016/j.avsg.2024.12.019
Effan Fahri Mahendra, R., & Burhan, A. (2024). The Effect of Aloe Vera Hydrogel on the Process of Burn Healing: A Systematic Review and Meta-Analysis. Journal of Wound Research and Technology, 1(1), 9–18. https://doi.org/10.70196/jwrt.v1i1.3
Effan Fahri Mahendra, R., Burhan, A., & Susanti, I. (2024). An analysis of various wound washing methods and their efficacy in treating chronic wounds: A comprehensive review of existing literature. Journal of Wound Research and Technology, 1(1), 1–8. https://doi.org/10.70196/jwrt.v1i1.2
Eid, M. A., et al. (2023). The global burden of peripheral artery disease. Journal of Vascular Surgery, 77(1), 285–296.e2. https://doi.org/10.1016/j.jvs.2022.10.030
Fine, J. P., & Gray, R. J. (1999). A proportional hazards model for the subdistribution of a competing risk. Journal of the American Statistical Association, 94(446), 496–509. https://doi.org/10.1080/01621459.1999.10474144
Fitridge, R., Chuter, V. H., Mills, J. L., Hinchliffe, R. J., Azuma, N., Behrendt, C.-A., et al. (2023). The intersocietal IWGDF, ESVS, SVS guidelines on PAD in diabetes with foot ulcer. Journal of Vascular Surgery, 78(6), 2108–2121. https://doi.org/10.1016/j.jvs.2023.09.004
Harrell, F. E. (2015). Regression modeling strategies (2nd ed.). Springer. https://doi.org/10.1007/978-3-319-19425-7
Hernán, M. A., & Robins, J. M. (2020). Causal inference: What if. Chapman & Hall/CRC.
International Working Group on the Diabetic Foot (IWGDF). (2023). IWGDF guideline on peripheral artery disease in diabetes (2023 update). https://iwgdfguidelines.org/wp-content/uploads/2023/07/IWGDF-2023-05-PAD-Guideline.pdf
International Working Group on the Diabetic Foot (IWGDF). (2023). Practical guidelines on the prevention and management of the diabetic foot (2023 update). https://iwgdfguidelines.org/wp-content/uploads/2023/07/IWGDF-2023-01-Practical-Guidelines.pdf
Kim, M. S., et al. (2023). Global burden of peripheral artery disease and its risk factors, 1990–2019. The Lancet Global Health, 11(10), e1601–e1613. https://doi.org/10.1016/S2214-109X(23)00355-8
Laird, N. M., & Ware, J. H. (1982). Random-effects models for longitudinal data. Biometrics, 38(4), 963–974. https://doi.org/10.2307/2529876
Lévesque, L. E., Hanley, J. A., & Kezouh, A. (2010). Problem of immortal time bias in cohort studies: Example using statins for preventing mortality in COPD. BMJ, 340, b5087. https://doi.org/10.1136/bmj.b5087
Lo, T., et al. (2009). Prediction of wound healing outcome using skin perfusion pressure and transcutaneous oxygen tension. International Wound Journal, 6(4), 330–337.
López-Moral, M., et al. (2023). Analyses of transcutaneous oxygen pressure values by angiosome for healing prognosis in diabetic foot ulcers. Diabetes Research and Clinical Practice, 205, 110781. https://doi.org/10.1016/j.diabres.2023.110781
Mixrova Sebayang, S., & Burhan, A. (2024). Comparison of Effectiveness of Hydropobic Cutimed Sorbact Versus Cadexomer Iodine 0.9% on Healing of Diabetic Foot Ulcer: A Randomized Control Trial. Journal of Wound Research and Technology, 1(1), 28–37. https://doi.org/10.70196/jwrt.v1i1.5
Ndosi, M., et al. (2017). Prognosis of the infected diabetic foot ulcer: A 12-month prospective observational study. Diabetic Medicine, 34(1), 78–88. https://doi.org/10.1111/dme.13270
Peduzzi, P., Concato, J., Kemper, E., Holford, T. R., & Feinstein, A. R. (1995). A simulation study of the number of events per variable in logistic regression analysis. Journal of Clinical Epidemiology, 48(12), 1373–1379. k
Račytė, A., et al. (2024). Oxygen saturation increase in ischemic wound tissues following revascularization. Sensors, 24(2), 582. https://doi.org/10.3390/s24020582
Rizopoulos, D. (2012). Joint models for longitudinal and time-to-event data: With applications in R. Chapman & Hall/CRC.
Royston, P., & Sauerbrei, W. (2008). Multivariable model-building. Wiley.
Society for Vascular Surgery (SVS). (2025). Patients with chronic limb-threatening ischemia (CLTI): Evidence-based guidance. https://vascular.org/patients-and-referring-physicians/referring-physicians/who-refer/patients-chronic-limb-threatening
Senneville, É., et al. (2023). IWGDF/IDSA guidelines on the diagnosis and treatment of foot infection in persons with diabetes. Clinical Infectious Diseases. https://doi.org/10.1093/cid/ciad527
Vickers, A. J., & Elkin, E. B. (2006). Decision curve analysis: A novel method for evaluating prediction models. Medical Decision Making, 26(6), 565–574. https://doi.org/10.1177/0272989X06295361
Vickers, A. J., van Calster, B., & Steyerberg, E. W. (2019). A simple, step-by-step guide to interpreting decision curve analysis. Diagnostic and Prognostic Research, 3, 18. https://doi.org/10.1186/s41512-019-0064-7
Wang, Z., Hasan, R., Firwana, B., et al. (2016). Tests to predict healing in the diabetic foot: A systematic review and meta-analysis. Journal of Vascular Surgery, 63(2 Suppl), 29S–36S.e2. https://doi.org/10.1016/j.jvs.2015.10.026
White, I. R., Royston, P., & Wood, A. M. (2011). Multiple imputation using chained equations: Issues and guidance for practice. Statistics in Medicine, 30(4), 377–399. https://doi.org/10.1002/sim.4067
Willems, S. A., et al. (2025). Prognostic performance of bedside tests for predicting ulcer healing and minor amputation outcomes. Diabetes/Metabolism Research and Reviews. Advance online publication. Vasc Med. 2025 Apr;30(2):250-260, https://doi.org/10.1177/1358863X241309326
Zagzoog, M., et al. (2025). Exercise TcPO₂ and outcomes after revascularization in intermittent claudication. Annals of Vascular Surgery. Advance online publication. https://doi.org/10.1016/j.avsg.2024.11.012
Zingg, M., et al. (2019). Transcutaneous oxygen pressure values often fail to predict stump failures after foot or limb amputation in chronically ischemic patients. Clinics in Surgery, 4, 2504. https://www.clinicsinsurgery.com/open-access/transcutaneous-oxygen-pressure-values-often-fail-to-predict-stump-failures-after-foot-or-limb-amputation-in-chronically-ischemic-patients-3780.pdf
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Kawamura Haruka, Asmat Burhan, Inoue Nanami, Fujita Kento

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.